Easy Methods To Combat Pes Planus
Overview

Most infants exhibit flat feet, but this is normal since most infants still have baby fat, which hides the arch formation. As the child grows and learns to walk, the soft tissues in the foot begin to tighten and form the arch. In most cases, the child will grow out of the condition and develop an arch before reaching adolescence. It?s important to remember that the muscles, bones, tendons, and ligaments are still in development. Children who complain of pain and have flat feet may suffer from a condition known as tarsal coalition. Tarsal coalition occurs when two or more bones in the foot fuse together. This causes great pain while walking, and shoes with arches are not helpful and can make the condition worse.
Causes
There is a lack of normal arch development, probably due to inherent ligamentous laxity. Around 20% of adults have Pes planus. The majority have a flexible flat foot and no symptoms. However, if there is also heel cord contracture, there may be symptoms (see 'Contributing factors', below). Loss of support for the arch. Dysfunction of the tibialis posterior tendon, a common and important cause. Tear of the spring ligament (rare). Tibialis anterior rupture (rare). A neuropathic foot, e.g from diabetes, polio, or other neuropathies. Degenerative changes in foot and ankle joints. Inflammatory arthropathy, eg rheumatoid arthritis. Osteoarthritis. Fractures. Bony abnormalities, eg tarsal coalition.
Symptoms
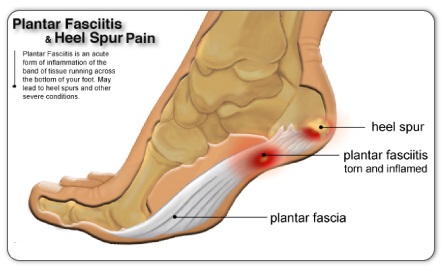
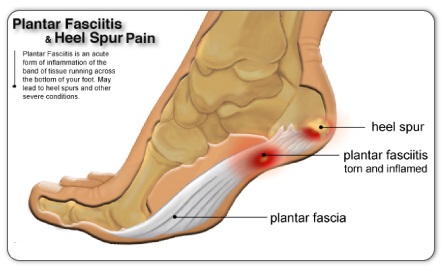
Knee/Hip/Back Pain - When the arch collapses in the foot, it triggers a series of compensations up the joint chain, leading to increased stress on the knee, pelvis and low back. Plantar fasciitis - This condition is characterized by heel pain, especially with the first few steps you take. The plantar fascia stretches as the arch falls, putting stress on the heel. Bunions - If you see a bony bump developing at the base of your big toe, you are likely developing a bunion. It may be swollen, red or painful when it rubs against your shoe. A flattened arch spreads the forefoot and causes the big toe to deviate toward the second toe. Shin splints - This term generally refers to pain anywhere along the shinbone. It is typically due to overuse and is aggravated after exercise and activity.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
What causes flat foot deformity?
Non Surgical Treatment
Heel cord stretching is an important part of treatment, as a tight Achilles tendon tends to pronate the foot. Orthotics (inserts or insoles, often custom-made) may be used. These usually contain a heel wedge to correct calcaneovalgus deformity, and an arch support. This is the usual treatment for flexible Pes Planus (if treatment is needed). A suitable insole can help to correct the deformity while it is worn. Possibly it may prevent progression of flat feet, or may reduce symptoms. However, the effectiveness of arch support insoles is uncertain. Arch supports used without correcting heel cord contracture can make symptoms worse. In patients with fixed Pes planus or arthropathy, customised insoles may relieve symptoms. Reduce contributing factors, wear shoes with low heels and wide toes. Lose weight if appropriate. Do exercises to strengthen foot muscles - walking barefoot (if appropriate), toe curls (flexing toes) and heel raises (standing on tiptoe).
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer).
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.

Most infants exhibit flat feet, but this is normal since most infants still have baby fat, which hides the arch formation. As the child grows and learns to walk, the soft tissues in the foot begin to tighten and form the arch. In most cases, the child will grow out of the condition and develop an arch before reaching adolescence. It?s important to remember that the muscles, bones, tendons, and ligaments are still in development. Children who complain of pain and have flat feet may suffer from a condition known as tarsal coalition. Tarsal coalition occurs when two or more bones in the foot fuse together. This causes great pain while walking, and shoes with arches are not helpful and can make the condition worse.
Causes
There is a lack of normal arch development, probably due to inherent ligamentous laxity. Around 20% of adults have Pes planus. The majority have a flexible flat foot and no symptoms. However, if there is also heel cord contracture, there may be symptoms (see 'Contributing factors', below). Loss of support for the arch. Dysfunction of the tibialis posterior tendon, a common and important cause. Tear of the spring ligament (rare). Tibialis anterior rupture (rare). A neuropathic foot, e.g from diabetes, polio, or other neuropathies. Degenerative changes in foot and ankle joints. Inflammatory arthropathy, eg rheumatoid arthritis. Osteoarthritis. Fractures. Bony abnormalities, eg tarsal coalition.
Symptoms
Knee/Hip/Back Pain - When the arch collapses in the foot, it triggers a series of compensations up the joint chain, leading to increased stress on the knee, pelvis and low back. Plantar fasciitis - This condition is characterized by heel pain, especially with the first few steps you take. The plantar fascia stretches as the arch falls, putting stress on the heel. Bunions - If you see a bony bump developing at the base of your big toe, you are likely developing a bunion. It may be swollen, red or painful when it rubs against your shoe. A flattened arch spreads the forefoot and causes the big toe to deviate toward the second toe. Shin splints - This term generally refers to pain anywhere along the shinbone. It is typically due to overuse and is aggravated after exercise and activity.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
What causes flat foot deformity?
Non Surgical Treatment
Heel cord stretching is an important part of treatment, as a tight Achilles tendon tends to pronate the foot. Orthotics (inserts or insoles, often custom-made) may be used. These usually contain a heel wedge to correct calcaneovalgus deformity, and an arch support. This is the usual treatment for flexible Pes Planus (if treatment is needed). A suitable insole can help to correct the deformity while it is worn. Possibly it may prevent progression of flat feet, or may reduce symptoms. However, the effectiveness of arch support insoles is uncertain. Arch supports used without correcting heel cord contracture can make symptoms worse. In patients with fixed Pes planus or arthropathy, customised insoles may relieve symptoms. Reduce contributing factors, wear shoes with low heels and wide toes. Lose weight if appropriate. Do exercises to strengthen foot muscles - walking barefoot (if appropriate), toe curls (flexing toes) and heel raises (standing on tiptoe).
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer).
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
All You Ought To Know About
Overview
Heel pain is a very common foot problem. The sufferer usually feels pain either under the heel (planter fasciitis) or just behind it (Achilles tendinitis), where the Achilles tendon connects to the heel bone. Even though heel pain can be severe and sometimes disabling, it is rarely a health threat. Heel pain is typically mild and usually disappears on its own; however, in some cases the pain may persist and become chronic (long-term). There are 26 bones in the human foot, of which the heel (calcaneus) is the largest. The human heel is designed to provide a rigid support for the weight of the body. When we are walking or running it absorbs the impact of the foot when it hits the ground, and springs us forward into our next stride. Experts say that the stress placed on a foot when walking may be 1.25 times our body weight, and 2.75 times when running. Consequently, the heel is vulnerable to damage, and ultimately pain.
Causes
The two major causes of heel pain are plantar fasciitis and achilles tendinitis. The easiest way to figure out which one is causing your pain is by location. Generally speaking, if the pain is under your heel bone it is likely plantar fasciitis. If the pain is found at the back of the heel, in the achilles or toward the base of the achilles (the long cord that extends from your calf to your heel bone), then it is likely achilles tendinitis.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
Depending on the condition, the cause of heel pain is diagnosed using a number of tests, including medical history, physical examination, including examination of joints and muscles of the foot and leg, X-rays.
Non Surgical Treatment
Treatment of heel pain generally occurs in stages. At the earliest sign of heel pain, aggressive calf muscle stretching should be started. Additionally, taking an oral anti-inflammatory medication and over-the- counter arch supports or heel cushions may be beneficial. The next phase of treatment might consist of continued calf muscle stretching exercises, cortisone injections and orthopedic taping of the foot to support the arch. If this treatment fails, or if there is reoccurrence of the heel pain, then functional foot orthotics might be considered. A functional orthotic is a device that is prescribed and fitted by your foot doctor, which fits in normal shoes like an arch support. Unlike an arch support, however the orthotic corrects abnormal pronation of the subtalar joint. Thus orthotics address the cause of the heel pain - abnormal pronation of the foot. Pump bump, treatment is similar to the treatment of bursitis and heel spurs. In rare cases, the bony growth at the heel may need to be removed surgically. Heel bruises can be treated by applying an ice pack for the first few minutes after injury. Achilles tendonitis, this condition is treated conservatively with rest, NSAIDs and physical therapy. If a sprain, fracture or other injury has caused the trapped nerve, this underlying problem must be treated first. In rare cases, surgery may be done to release the trapped nerve.
Surgical Treatment
With the advancements in technology and treatments, if you do need to have surgery for the heel, it is very minimal incision that?s done. And the nice thing is your recovery period is short and you should be able to bear weight right after the surgery. This means you can get back to your weekly routine in just a few weeks. Recovery is a lot different than it used to be and a lot of it is because of doing a minimal incision and decreasing trauma to soft tissues, as well as even the bone. So if you need surgery, then your recovery period is pretty quick.
foot pain heel
Prevention

Wear properly fitting shoes. Place insoles or inserts in your shoes to help control abnormal foot motion. Maintain a healthy weight. Exercise and do foot stretches as they have been shown to decrease the incidence of heel pain.
Heel pain is a very common foot problem. The sufferer usually feels pain either under the heel (planter fasciitis) or just behind it (Achilles tendinitis), where the Achilles tendon connects to the heel bone. Even though heel pain can be severe and sometimes disabling, it is rarely a health threat. Heel pain is typically mild and usually disappears on its own; however, in some cases the pain may persist and become chronic (long-term). There are 26 bones in the human foot, of which the heel (calcaneus) is the largest. The human heel is designed to provide a rigid support for the weight of the body. When we are walking or running it absorbs the impact of the foot when it hits the ground, and springs us forward into our next stride. Experts say that the stress placed on a foot when walking may be 1.25 times our body weight, and 2.75 times when running. Consequently, the heel is vulnerable to damage, and ultimately pain.
Causes
The two major causes of heel pain are plantar fasciitis and achilles tendinitis. The easiest way to figure out which one is causing your pain is by location. Generally speaking, if the pain is under your heel bone it is likely plantar fasciitis. If the pain is found at the back of the heel, in the achilles or toward the base of the achilles (the long cord that extends from your calf to your heel bone), then it is likely achilles tendinitis.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
Depending on the condition, the cause of heel pain is diagnosed using a number of tests, including medical history, physical examination, including examination of joints and muscles of the foot and leg, X-rays.
Non Surgical Treatment
Treatment of heel pain generally occurs in stages. At the earliest sign of heel pain, aggressive calf muscle stretching should be started. Additionally, taking an oral anti-inflammatory medication and over-the- counter arch supports or heel cushions may be beneficial. The next phase of treatment might consist of continued calf muscle stretching exercises, cortisone injections and orthopedic taping of the foot to support the arch. If this treatment fails, or if there is reoccurrence of the heel pain, then functional foot orthotics might be considered. A functional orthotic is a device that is prescribed and fitted by your foot doctor, which fits in normal shoes like an arch support. Unlike an arch support, however the orthotic corrects abnormal pronation of the subtalar joint. Thus orthotics address the cause of the heel pain - abnormal pronation of the foot. Pump bump, treatment is similar to the treatment of bursitis and heel spurs. In rare cases, the bony growth at the heel may need to be removed surgically. Heel bruises can be treated by applying an ice pack for the first few minutes after injury. Achilles tendonitis, this condition is treated conservatively with rest, NSAIDs and physical therapy. If a sprain, fracture or other injury has caused the trapped nerve, this underlying problem must be treated first. In rare cases, surgery may be done to release the trapped nerve.
Surgical Treatment
With the advancements in technology and treatments, if you do need to have surgery for the heel, it is very minimal incision that?s done. And the nice thing is your recovery period is short and you should be able to bear weight right after the surgery. This means you can get back to your weekly routine in just a few weeks. Recovery is a lot different than it used to be and a lot of it is because of doing a minimal incision and decreasing trauma to soft tissues, as well as even the bone. So if you need surgery, then your recovery period is pretty quick.
foot pain heel
Prevention

Wear properly fitting shoes. Place insoles or inserts in your shoes to help control abnormal foot motion. Maintain a healthy weight. Exercise and do foot stretches as they have been shown to decrease the incidence of heel pain.
Leg Length Discrepancy Gait
Overview
Surgical options in leg length discrepancy treatment include procedures to lengthen the shorter leg, or shorten the longer leg. Your child's physician will choose the safest and most effective method based on the aforementioned factors. No matter the surgical procedure performed, physical therapy will be required after surgery in order to stretch muscles and help support the flexibility of the surrounding joints. Surgical shortening is safer than surgical lengthening and has fewer complications. Surgical procedures to shorten one leg include removing part of a bone, called a bone resection. They can also include epiphysiodesis or epiphyseal stapling, where the growth plate in a bone is tethered or stapled. This slows the rate of growth in the surgical leg.
Causes
There are many causes of leg length discrepancy. Structural inequality is due to interference of normal bone growth of the lower extremity, which can occur from trauma or infection in a child. Functional inequality has many causes, including Poliomyelitis or other paralytic deformities can retard bone growth in children. Contracture of the Iliotibial band. Scoliosis or curvature of the spine. Fixed pelvic obliquity. Abduction or flexion contraction of the hip. Flexion contractures or other deformities of the knee. Foot deformities.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
The doctor carefully examines the child. He or she checks to be sure the legs are actually different lengths. This is because problems with the hip (such as a loose joint) or back (scoliosis) can make the child appear to have one shorter leg, even though the legs are the same length. An X-ray of the child?s legs is taken. During the X-ray, a long ruler is put in the image so an accurate measurement of each leg bone can be taken. If an underlying cause of the discrepancy is suspected, tests are done to rule it out.
Non Surgical Treatment
Internal heel lifts: Putting a simple heel lift inside the shoe or onto a foot orthotic has the advantage of being transferable to many pairs of shoes. It is also aesthetically more pleasing as the lift remains hidden from view. However, there is a limit as to how high the lift can be before affecting shoe fit. Dress shoes will usually only accommodate small lifts (1/8"1/4") before the heel starts to piston out of the shoe. Sneakers and workboots may allow higher lifts, e.g., up to 1/2", before heel slippage problems arise. External heel lifts: If a lift of greater than 1/2" is required, you should consider adding to the outsole of the shoe. In this way, the shoe fit remains good. Although some patients may worry about the cosmetics of the shoe, it does ensure better overall function. Nowadays with the development of synthetic foams and crepes, such lifts do not have to be as heavy as the cork buildups of the past. External buildups are not transferable and they will wear down over time, so the patient will need to be vigilant in having them repaired. On ladies' high-heel shoes, it may be possible to lower one heel and thereby correct the imbalance.

how to grow taller fast in a week
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
Surgical options in leg length discrepancy treatment include procedures to lengthen the shorter leg, or shorten the longer leg. Your child's physician will choose the safest and most effective method based on the aforementioned factors. No matter the surgical procedure performed, physical therapy will be required after surgery in order to stretch muscles and help support the flexibility of the surrounding joints. Surgical shortening is safer than surgical lengthening and has fewer complications. Surgical procedures to shorten one leg include removing part of a bone, called a bone resection. They can also include epiphysiodesis or epiphyseal stapling, where the growth plate in a bone is tethered or stapled. This slows the rate of growth in the surgical leg.

Causes
There are many causes of leg length discrepancy. Structural inequality is due to interference of normal bone growth of the lower extremity, which can occur from trauma or infection in a child. Functional inequality has many causes, including Poliomyelitis or other paralytic deformities can retard bone growth in children. Contracture of the Iliotibial band. Scoliosis or curvature of the spine. Fixed pelvic obliquity. Abduction or flexion contraction of the hip. Flexion contractures or other deformities of the knee. Foot deformities.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
The doctor carefully examines the child. He or she checks to be sure the legs are actually different lengths. This is because problems with the hip (such as a loose joint) or back (scoliosis) can make the child appear to have one shorter leg, even though the legs are the same length. An X-ray of the child?s legs is taken. During the X-ray, a long ruler is put in the image so an accurate measurement of each leg bone can be taken. If an underlying cause of the discrepancy is suspected, tests are done to rule it out.
Non Surgical Treatment
Internal heel lifts: Putting a simple heel lift inside the shoe or onto a foot orthotic has the advantage of being transferable to many pairs of shoes. It is also aesthetically more pleasing as the lift remains hidden from view. However, there is a limit as to how high the lift can be before affecting shoe fit. Dress shoes will usually only accommodate small lifts (1/8"1/4") before the heel starts to piston out of the shoe. Sneakers and workboots may allow higher lifts, e.g., up to 1/2", before heel slippage problems arise. External heel lifts: If a lift of greater than 1/2" is required, you should consider adding to the outsole of the shoe. In this way, the shoe fit remains good. Although some patients may worry about the cosmetics of the shoe, it does ensure better overall function. Nowadays with the development of synthetic foams and crepes, such lifts do not have to be as heavy as the cork buildups of the past. External buildups are not transferable and they will wear down over time, so the patient will need to be vigilant in having them repaired. On ladies' high-heel shoes, it may be possible to lower one heel and thereby correct the imbalance.

how to grow taller fast in a week
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
What Causes Mortons Neuroma
Overview
 Morton?s neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton?s neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton?s neuroma is 8 to 10 times greater in women than in men.
Morton?s neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton?s neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton?s neuroma is 8 to 10 times greater in women than in men.
Causes
There are a number of common causes for Morton?s Neuroma, (though the condition can arise spontaneously for reasons still unknown). The Neuroma often occurs in response to irritation, pressure or traumatic injury to one of the digital nerves leading to the toes. A thickening of nerve tissue results as part of the body?s response to the irritation or injury. Abnormal foot movement used to compensate for bunions, hammertoes, flatfeet and other conditions can lead to irritation and development of Morton?s Neuroma. Pronation of the foot may cause the heads of the metatarsal bones to rotate slightly, thereby pinching the nerve running between the metatarsal heads. Chronic pressure or pinching causes the nerve sheath to enlarge, becoming increasingly squeezed, producing worsening pain over time, if not addressed. Morton?s Neuroma can be exacerbated when tight shoes providing little room for the forefoot are worn. Activities which over-pronate the foot (such as walking barefoot in sand) may increase the pain associated with Morton?s Neuroma, as will any high-impact activity, such as jogging.
Symptoms
Patients will often experience a clicking feeling in the forefoot followed by a sharp shooting pain or a sensation of numbness or pins and needles extending into ends of their toes. Tight narrow fitting shoes may often exacerbate these feelings which become worse after long periods of standing or walking. Once the Mortons nueroma progresses symptoms will become more frequent and often more intense.
Diagnosis
Patients with classic Morton?s neuroma symptoms will have pain with pressure at the base of the involved toes (either between the 2nd and 3rd toes, or between the 3rd and 4th toes). In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe as this corresponds with the distribution of the involved nerve.
Non Surgical Treatment
Initial therapies are nonsurgical and relatively simple. They can involve one or more of the following treatments. Changes in footwear. Avoid high heels or tight shoes, and wear wider shoes with lower heels and a soft sole. This enables the bones to spread out and may reduce pressure on the nerve, giving it time to heal. Orthoses. Custom shoe inserts and pads also help relieve irritation by lifting and separating the bones, reducing the pressure on the nerve. Injection. One or more injections of a corticosteroid medication can reduce the swelling and inflammation of the nerve, bringing some relief. Several studies have shown that a combination of roomier, more comfortable shoes, nonsteroidal anti-inflammatory medication, custom foot orthoses and cortisone injections provide relief in over 80 percent of people with Morton's Neuroma.
Surgical Treatment
Patients are commonly offered surgery known as neurectomy, which involves removing the affected piece of nerve tissue. Postoperative scar tissue formation (known as stump neuroma) can occur in approximately 20%-30% of cases, causing a return of neuroma symptoms. Neurectomy can be performed using one of two general methods. Making the incision from the dorsal side (the top of the foot) is the more common method but requires cutting the deep transverse metatarsal ligament that connects the 3rd and 4th metatarsals in order to access the nerve beneath it. This results in exaggerated postoperative splaying of the 3rd and 4th digits (toes) due to the loss of the supporting ligamentous structure. This has aesthetic concerns for some patients and possible though unquantified long-term implications for foot structure and health. Alternatively, making the incision from the ventral side (the sole of the foot) allows more direct access to the affected nerve without cutting other structures. However, this approach requires a greater post-operative recovery time where the patient must avoid weight bearing on the affected foot because the ventral aspect of the foot is more highly enervated and impacted by pressure when standing. It also has an increased risk that scar tissue will form in a location that causes ongoing pain.
 Morton?s neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton?s neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton?s neuroma is 8 to 10 times greater in women than in men.
Morton?s neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton?s neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton?s neuroma is 8 to 10 times greater in women than in men.Causes
There are a number of common causes for Morton?s Neuroma, (though the condition can arise spontaneously for reasons still unknown). The Neuroma often occurs in response to irritation, pressure or traumatic injury to one of the digital nerves leading to the toes. A thickening of nerve tissue results as part of the body?s response to the irritation or injury. Abnormal foot movement used to compensate for bunions, hammertoes, flatfeet and other conditions can lead to irritation and development of Morton?s Neuroma. Pronation of the foot may cause the heads of the metatarsal bones to rotate slightly, thereby pinching the nerve running between the metatarsal heads. Chronic pressure or pinching causes the nerve sheath to enlarge, becoming increasingly squeezed, producing worsening pain over time, if not addressed. Morton?s Neuroma can be exacerbated when tight shoes providing little room for the forefoot are worn. Activities which over-pronate the foot (such as walking barefoot in sand) may increase the pain associated with Morton?s Neuroma, as will any high-impact activity, such as jogging.
Symptoms
Patients will often experience a clicking feeling in the forefoot followed by a sharp shooting pain or a sensation of numbness or pins and needles extending into ends of their toes. Tight narrow fitting shoes may often exacerbate these feelings which become worse after long periods of standing or walking. Once the Mortons nueroma progresses symptoms will become more frequent and often more intense.
Diagnosis
Patients with classic Morton?s neuroma symptoms will have pain with pressure at the base of the involved toes (either between the 2nd and 3rd toes, or between the 3rd and 4th toes). In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe as this corresponds with the distribution of the involved nerve.
Non Surgical Treatment
Initial therapies are nonsurgical and relatively simple. They can involve one or more of the following treatments. Changes in footwear. Avoid high heels or tight shoes, and wear wider shoes with lower heels and a soft sole. This enables the bones to spread out and may reduce pressure on the nerve, giving it time to heal. Orthoses. Custom shoe inserts and pads also help relieve irritation by lifting and separating the bones, reducing the pressure on the nerve. Injection. One or more injections of a corticosteroid medication can reduce the swelling and inflammation of the nerve, bringing some relief. Several studies have shown that a combination of roomier, more comfortable shoes, nonsteroidal anti-inflammatory medication, custom foot orthoses and cortisone injections provide relief in over 80 percent of people with Morton's Neuroma.

Surgical Treatment
Patients are commonly offered surgery known as neurectomy, which involves removing the affected piece of nerve tissue. Postoperative scar tissue formation (known as stump neuroma) can occur in approximately 20%-30% of cases, causing a return of neuroma symptoms. Neurectomy can be performed using one of two general methods. Making the incision from the dorsal side (the top of the foot) is the more common method but requires cutting the deep transverse metatarsal ligament that connects the 3rd and 4th metatarsals in order to access the nerve beneath it. This results in exaggerated postoperative splaying of the 3rd and 4th digits (toes) due to the loss of the supporting ligamentous structure. This has aesthetic concerns for some patients and possible though unquantified long-term implications for foot structure and health. Alternatively, making the incision from the ventral side (the sole of the foot) allows more direct access to the affected nerve without cutting other structures. However, this approach requires a greater post-operative recovery time where the patient must avoid weight bearing on the affected foot because the ventral aspect of the foot is more highly enervated and impacted by pressure when standing. It also has an increased risk that scar tissue will form in a location that causes ongoing pain.
Why Shoe Lifts Are The Answer To Leg Length Imbalances
There are actually not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is anatomically shorter than the other. As a result of developmental phases of aging, the brain senses the stride pattern and identifies some difference. The body typically adapts by tilting one shoulder over to the "short" side. A difference of under a quarter inch isn't blatantly uncommon, doesn't need Shoe Lifts to compensate and normally won't have a serious effect over a lifetime.

Leg length inequality goes mainly undiagnosed on a daily basis, yet this issue is easily corrected, and can eliminate a number of instances of chronic back pain.
Treatment for leg length inequality usually involves Shoe Lifts. These are typically low-priced, in most cases being under twenty dollars, in comparison to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Mid back pain is easily the most widespread ailment impacting people today. Over 80 million men and women experience back pain at some stage in their life. It's a problem which costs employers millions each year due to lost time and output. Fresh and more effective treatment methods are always sought after in the hope of lowering economical influence this condition causes.

Men and women from all corners of the world experience foot ache due to leg length discrepancy. In a lot of these situations Shoe Lifts can be of immense help. The lifts are capable of decreasing any pain in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
So as to support the body in a balanced fashion, feet have a crucial part to play. Irrespective of that, it is sometimes the most overlooked zone of the human body. Many people have flat-feet which means there is unequal force placed on the feet. This causes other areas of the body like knees, ankles and backs to be impacted too. Shoe Lifts guarantee that correct posture and balance are restored.

Leg length inequality goes mainly undiagnosed on a daily basis, yet this issue is easily corrected, and can eliminate a number of instances of chronic back pain.
Treatment for leg length inequality usually involves Shoe Lifts. These are typically low-priced, in most cases being under twenty dollars, in comparison to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Mid back pain is easily the most widespread ailment impacting people today. Over 80 million men and women experience back pain at some stage in their life. It's a problem which costs employers millions each year due to lost time and output. Fresh and more effective treatment methods are always sought after in the hope of lowering economical influence this condition causes.

Men and women from all corners of the world experience foot ache due to leg length discrepancy. In a lot of these situations Shoe Lifts can be of immense help. The lifts are capable of decreasing any pain in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
So as to support the body in a balanced fashion, feet have a crucial part to play. Irrespective of that, it is sometimes the most overlooked zone of the human body. Many people have flat-feet which means there is unequal force placed on the feet. This causes other areas of the body like knees, ankles and backs to be impacted too. Shoe Lifts guarantee that correct posture and balance are restored.
What Is Posterior Calcaneal Spur

Overview
A heel spur is a deposit of calcium on the heel bone. This calcification takes the form of a bony protrusion, which can cause considerable pain when standing and walking. This foot problem is closely related to plantar fasciitis, a condition in which the band of fibrous tissue on the bottom of the foot becomes over-stressed. It pulls away from the heel and causes the calcium deposits to form. For this reason, treating a heel spur involves treating the plantar fascia as well.
Causes
A heel spur can develop when there is an abundance of calcium creating a deposit in the calcaneus, or heel bone. Over time, this deposit grows to create an outcropping under the heel that extends into the foot. The result is a protrusion that leads to foot pain when pressure is applied, and in some cases, even during rest.

Symptoms
Heel spurs may or may not cause symptoms. Symptoms are usually related to the plantar fasciitis. You may experience significant pain. Your heel pain may be worse in the morning when you first wake up or during certain activities.
Diagnosis
A heel spur is often seen on X-ray as a bony protrusion, which can vary in size. However, because a Heel Spur only indicates increased load on the plantar fascia, and not pain, an ultra sound may be required to assess other actual cause of the heel pain such and may include checking to see if the plantar fascia is inflamed or degenerated.
Non Surgical Treatment
There are both conservative and surgical heel spur treatment options. Because the heel pain caused by heel spurs is symptomatic of inflammation, the first step is to ice the area in hopes to reduce the inflammation. The next step is to see our orthopedic specialist to prescribe an appropriate treatment plan. Some conservative treatment options might include Anti-inflammatory medications. Shoe orthotics. Shoe inserts. If conservative treatments are not working, surgery may be required to remove the heel spur. As in all cases of heel pain, it is important to see an orthopedic doctor who specializes in foot and ankle pain.
Surgical Treatment
In a small number of cases (usually less than 5 percent), patients may not experience relief after trying the recommendations listed above. It is important that conservative treatments (such as those listed above) be performed for AT LEAST a year before considering surgery. Time is important in curing the pain from heel spurs, and insufficient treatment before surgery may subject you to potential complications from the procedure. If these treatments fail, your doctor may consider an operation to loosen the plantar fascia, called a plantar fascia release.
Prevention
The best way to prevent heel spurs is by wearing properly fitted footwear. Shoes should have a shock absorbing tread and soles and should be effective in supporting the heel and arch. Proper warm up and stretching before embarking on any physical activity that will put pressure or impact on the area is highly recommended. Also, just as it?s important for your general health, if you can lose some extra pounds, you will be more likely to avoid heel spurs. If you are starting to feel the onset of pain, it may not be heel spurs, but could be a tendonitis condition that could lead to heel spurs.
Learn How To Protect Against Inferior Calcaneal Spur

Overview
The two most common causes of pain in the bottom of the heel, the arch, or both the heel and the arch, are heel spurs and plantar fasciitis. A Heel Spur is a piece of calcium or bone that sticks out from the bottom of the heel bone, and lies within the fibers of the plantar fascia. When walking, the spur digs into the plantar fascia and causes small micro-tears in the plantar fascia. This produces inflammation and pain in the heel, which at times may radiate into the arch.
Causes
Causes of Heel Spur Syndrome are mostly due to your foot structure. Foot structure is due to hereditary for the most part, meaning it was the way you were when born. Other factors such as increase in weight, injury, improper shoes, or different activities may change the way your foot functions as well. If one leg is longer or shorter than the other, this may make your foot function improperly and be the cause of the heel spur syndrome. Improper shoes may be ones that are new or ones that are worn out and do not give good support. The higher priced shoes do not mean it's a better shoe. Pronation is a term used to describe a foot which allows the arch to fall more than normal and allows for the fascia along the bottom of the foot to put a tighter pull or a different angle of pull on the heel bone. Over time, this constant pull of the tight fascia can force the bone to enlarge and form a spur. It is not the heel spur that causes the pain directly. The spur may cause pressure against a nearby nerve causing a neuritis, or a bursa causing a bursitis.

Symptoms
More often than not, heel spurs have no signs or symptoms, and you don?t feel any pain. This is because heel spurs aren?t pointy or sharp pieces of bone, contrary to common belief. Heel spurs don?t cut tissue every time movement occurs; they?re actually deposits of calcium on bone set in place by the body?s normal bone-forming mechanisms. This means they?re smooth and flat, just like all other bones. Because there?s already tissue present at the site of a heel spur, sometimes that area and the surrounding tissue get inflamed, leading to a number of symptoms, such as chronic heel pain that occurs when jogging or walking.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
Conventional treatment for heel spurs typically includes rest, stretching exercises, icing and anti-inflammatory medications. Many people find it difficult to go through the day without some sort of routine activity or exercise, and this prolongs the heel spur and forces people to rely on anti-inflammatory medications for a longer period of time. This can be detrimental due to the many side effects of these medications, including gastrointestinal problems like leaky gut, bleeding and ulcer symptoms.
Surgical Treatment
Almost 90% of the people suffering from heel spur get better with nonsurgical treatments. However, if the conservative treatments do not help you and you still have pain even after 9 to 12 months, your doctor may advise surgery for treating heel spur. The surgery helps in reducing the pain and improving your mobility. Some of the surgical techniques used by doctors are release of the plantar fascia. Removal of a spur. Before the surgery, the doctor will go for some pre-surgical tests and exams. After the operation, you will need to follow some specific recommendations which may include elevation of the foot, waiting time only after which you can put weight on the foot etc.